Knee Osteoarthritis


Osteoarthritis
Osteoarthritis of the knee, also known as knee OA, is a degenerative joint disease that primarily affects the articular cartilage and surrounding structures in the knee joint. It is the most common form of arthritis and a leading cause of chronic pain and disability among older adults. Knee OA typically develops slowly over time due to the wear and tear on the joint, but it can also occur as a result of previous knee injuries or conditions that affect joint alignment.
In knee OA, the protective cartilage that covers the ends of the bones within the knee joint gradually deteriorates, leading to friction, inflammation, and damage to the underlying bone. This results in pain, stiffness, swelling, and reduced range of motion in the affected knee. As the disease progresses, bone spurs (osteophytes) may develop, further contributing to joint pain and dysfunction.
Knee OA is more common in individuals over the age of 50, although it can affect people of all ages. Certain risk factors increase the likelihood of developing knee OA, including obesity, previous knee injuries, repetitive stress on the knee joint, genetic factors, and conditions such as rheumatoid arthritis or gout.
The diagnosis of knee OA is typically based on a combination of clinical evaluation, medical history, physical examination findings, and imaging studies such as X-rays or MRI scans.
Treatment for knee OA aims to relieve pain, improve joint function, and enhance quality of life. It involves a combination of non-pharmacological interventions (e.g., weight management, exercise, physical therapy), pharmacological treatments (e.g., pain medications, anti-inflammatory drugs), and in some cases, surgical interventions (e.g., arthroscopy or joint replacement surgery).
Overall, osteoarthritis of the knee is a chronic condition that requires a comprehensive and multidisciplinary approach to manage effectively. Treatment plans are often individualized based on the severity of symptoms, impact on daily activities, and patient preferences. Regular monitoring and follow-up are essential to evaluate treatment effectiveness and modify management strategies as needed.
It is important to consult A/Prof Papantoniou to determine the best course of treatment for your specific case.
Total Knee Replacement

Total Knee Replacement: What to Expect
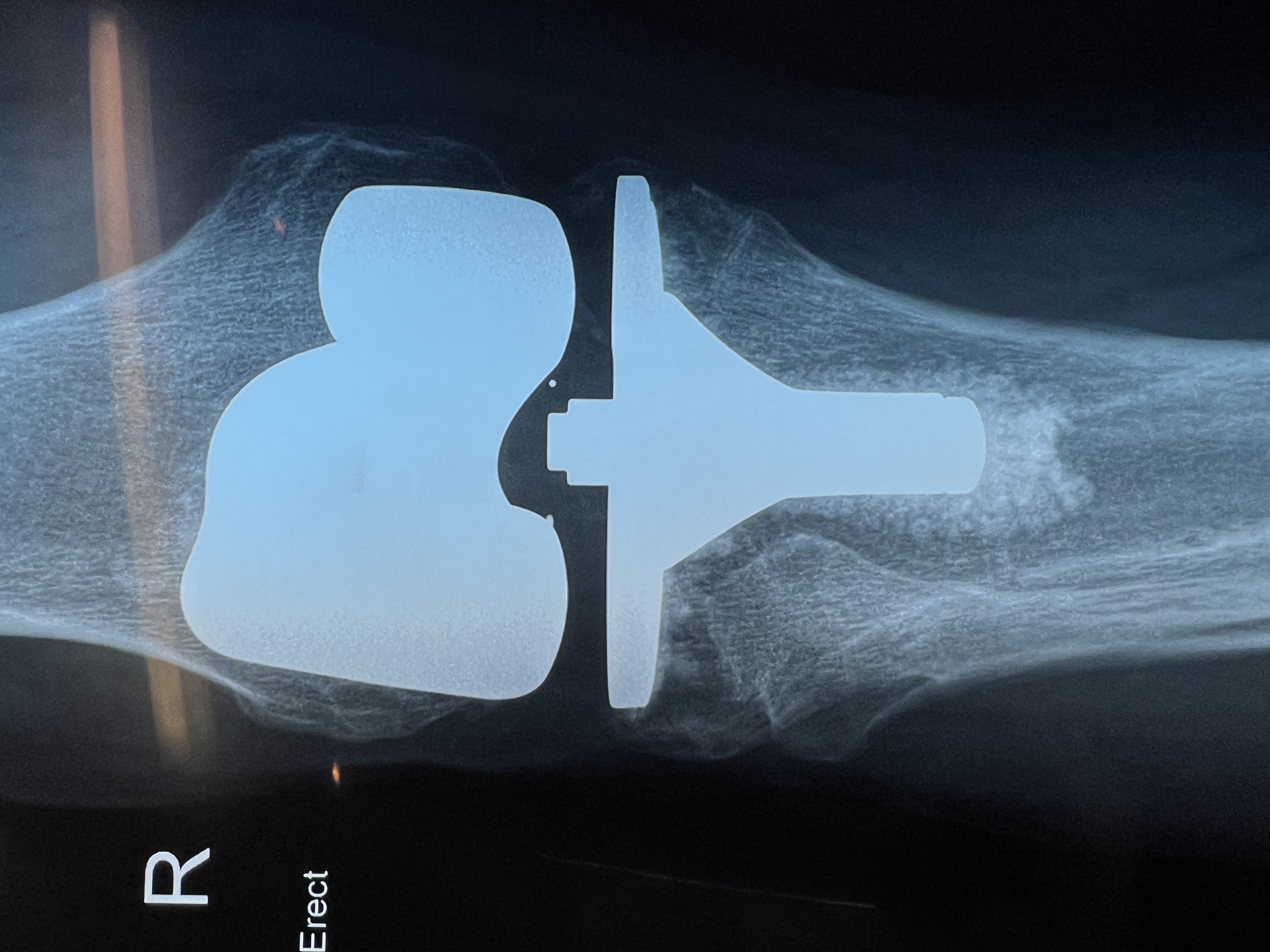
A total knee replacement is a surgery to replace a damaged or worn-out knee joint with an artificial one. It is often done for people with severe arthritis or injuries that cause chronic pain, stiffness, and difficulty walking.
How Is It Done?
The procedure is performed under general and spinal anaesthesia. A/Prof Papantoniou:
1. Removes the damaged bone and cartilage from the ends of the femur and tibia.
2. Shapes the bones to fit the artificial joint.
3. Attaches the new knee joint, made of metal and plastic, to restore smooth movement.
4. Tests for proper movement and stability before closing the incision.
Recovery & Rehabilitation
• Hospital stay: Overnight – most patients go home the next morning.
• Walking begins within a day with support.
• Physiotherapy is essential to regain strength and flexibility.
• Full recovery takes several months, though most people experience significant pain relief and improved mobility.
Is It Worth It?
A total knee replacement can restore independence and improve quality of life, allowing patients to return to normal activities without constant pain. Following post-surgery exercises and precautions is key to long-term success.