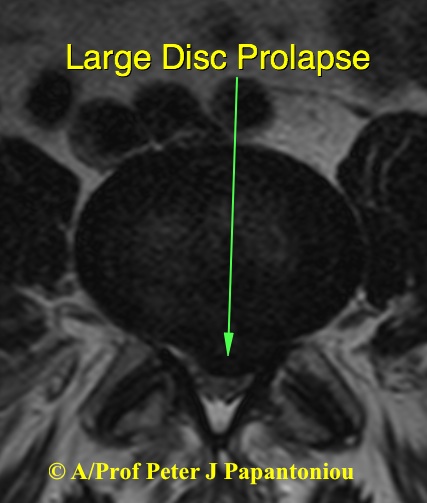

Disc Prolapse
A disc prolapse, also known as a herniated disc or slipped disc, occurs when the soft, spongy material (nucleus pulposus) inside a spinal disc bulges out through a crack in the tougher exterior (annulus fibrosis). This can put pressure on nearby nerves, causing pain and other symptoms such as tingling or numbness in the limbs.
The treatment for a disc prolapse typically depends on the severity of symptoms. Options may include conservative management, interventional procedures such as epidural steroid injections, and surgery (discectomy or fusion) for severe cases.
It is important to consult A/Prof Papantoniou to determine the best course of treatment for your specific case.
Lumbar Discectomy: What You Need to Know
A lumbar discectomy is a surgical procedure to remove part of a damaged or herniated disc in the lower spine. It relieves pressure on a spinal nerve, reducing pain, numbness, and weakness often caused by sciatica.
When Is It Needed?
- Severe leg pain persists despite non-surgical treatments.
- Weakness or numbness worsens.
- Bladder or bowel control is affected – a medical emergency.
How Is It Done?
The procedure is performed under general anesthesia with a small incision and minimally invasive or endoscopic techniques.
Recovery and Outlook
- Most patients go home the next day.
- Light activities resume in a few weeks; full recovery takes around 6 weeks.
- Physiotherapy is recommended to restore strength and prevent future issues.
A lumbar discectomy has a high success rate, but proper posture, exercise, and lifestyle changes are essential for long-term relief.